Long COVID: In the head or body?
A Dutch-led medical study is said to have found a physical cause for the disease. Can this be confirmed on closer inspection? And what does this mean for patients?
“People with long-COVID are still too often told: ‘It’s all in your head’. Unfortunately, we hear from patients that those around them, sometimes even their GP, still think it’s burnout. We hope that this research will help educate the public that it is a physical illness that people can do nothing about themselves.”
Comment on the new study by Diewke de Haen, director of the patient organization PostCovidNL
Even though COVID is increasingly becoming a “normal” illness like the annual viral flu, the pandemic is not over for everyone: some people experience significant health restrictions even months to years after being infected with the coronavirus. We call this “long COVID”.
A study just published in Nature Communications led by Dutch researchers at the University Medical Center Amsterdam now reports interesting results: After physical exertion, conspicuous changes were found in the muscle tissue of those affected. This mainly concerned the activity of the mitochondria, the power plants of the cells, so to speak, and certain protein deposits. If these accumulate, the state of health can even deteriorate.
For the study, 25 patients took part in a cycling performance test under controlled conditions. On average, they were 41 years old, with roughly equal numbers of men and women. There were 21 healthy people in the comparison group. In both groups, almost 100% of the people were vaccinated against COVID. However, the patients with long COVID were only able to work an average of five hours per week – compared to 36 before the disease.
Correlate or correlation?
In the Dutch media – and probably not only there – far-reaching conclusions were drawn:
“Long COVID has a physical cause. Researchers from the University Medical Center Amsterdam and the Free University have discovered this by examining muscle tissue from people with and without Long COVID.”
NOS.nl on January 4, 2024
This conclusion also serves as the title headline. However, if you look at the original study (open access), you will find a different conclusion: “This study is observational in nature, and therefore we cannot establish causality.” (p. 9).
This is by no means intended to relativize the effects found: The differences in amyloid deposits – certain proteins in the muscles – can be very large.
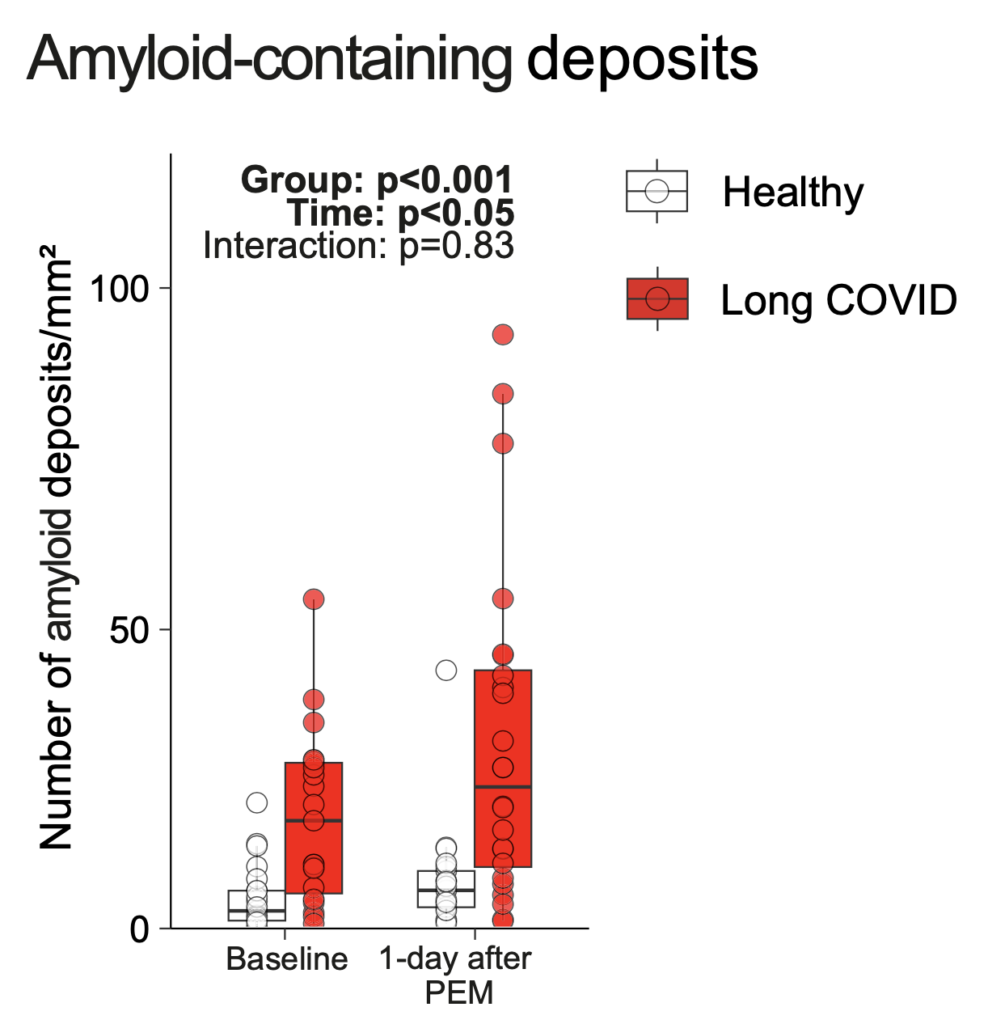
Figure: On average, the differences in deposits between patients with long COVID and the healthy comparison subjects are significant. However, a look at the data also shows large overlaps between the two groups. Source: Appelman et al., 2024. License: CC BY 4.0 DEED
You can see that many of the patients – before and after the performance test – show no different amount of deposits. This means that the test can only be a biological indication of long COVID, but certainly not proof of its presence or cause. And for principal reasons.
It is a statistical correlation, not “the correlate” of the disease. Unfortunately, this confusion happens very often in science and science communication.
Extreme conclusions
Just as extreme and nonsensical as the claim that long COVID is purely psychological is the extreme exaggeration that the disease is purely physical and there is nothing patients can do about it.
It may be that some of those affected were tormented with physiotherapy and other training that overtaxed them and perhaps even worsened their state of health. However, this is above all an expression of bureaucratic medicine in which treatment protocols are stubbornly followed.
Accordingly, doctor and researcher Brent Appelman, one of the main authors of the new study, recommends taking individual physical limits into account during therapy. Interestingly, he literally puts the responsibility for this on the patients themselves – typical Dutch mentality:
“Specifically, we advise these patients to pay attention to their physical limits and not to exceed them. Think of light exertion that does not lead to a worsening of the symptoms. To maintain physical condition, it is good to go for a walk or ride an electric bike. It should be borne in mind that every patient has a different exercise tolerance.”
Brent Appelman from the University Medical Center Amsterdam
This alone contradicts the statement by Diewke de Haen, director of the patient organization PostCovidNL, quoted at the beginning. With this extreme one-sidedness, she may be harming those affected herself if they now exercise less. The misconception that people with depression have a brain disease and cannot do anything about it has already proven to be similarly harmful.
Body and soul
The reports also show that dualistic thinking is still prevalent in many people’s minds centuries after René Descartes (1596-1650). Body and soul, body and mind are therefore strongly separated from each other. Yet for us, the two form an inseparable unity – or are simply different perspectives on the same thing. As I said years ago: body is mind.
In particular, it does not make a problem any less real, even if it is primarily psychological or psychosomatic. People who think this way have completely lost touch with themselves. Because even the body, which is supposedly so much more real, is conveyed to us in our experience: it is something other than a chair we sit on or a fork we eat with; it is rather a living, organic, even “ensouled” body.
In this way, we see how a confused mind-body philosophy is not only up to mischief on paper, but can actually harm people. We constantly experience the embodiment of our psychological life when, for example, we drink a glass of alcohol to relieve stress or embarrassment. (Interestingly, the effect of psychoactive substances in itself depends on our expectations; set and setting).
Conversely, changes in the immune system or other parts of the body can sometimes be found in people with depression. Or people with attention deficit disorder can sometimes concentrate better after a sports session.
A good physiotherapist will also ask their clients about their mental well-being: How is their sleep? Does someone have a lot of stress? Major psychosocial problems? Such factors can cause physical problems or at least contribute to their occurrence. And they are always important for the recovery process.
Recommendations
The discussion as to whether long COVID is physical, psychosomatic or psychological is therefore as pointless as the eternal dispute as to whether certain mental abilities are innate or acquired (nature or nurture). Culture has become second nature to us humans. And in a certain sense, almost all our physical problems are psychosomatic, if only because our attitude and behavior influence our recovery. Just think of placebo and nocebo effects.
In this respect, it is better not to follow the conclusion of the patient organization that nothing can be done about long COVID. If you do, you are giving away the potential of your body’s self-healing powers, however small they may be in individual cases.
It is a truism that individual possibilities must be taken into account when it comes to exercise and lifestyle. If this has gone wrong too often, as the reports now suggest, this is a further indication of the sickness of our healthcare system with its bureaucracy and excessive standardization of treatment protocols.
We could also reconsider whether “long COVID” is the best term: COVID is primarily an infectious viral respiratory disease. This can also affect other organs and systems, as the new study once again confirms. However, chronic patients usually no longer suffer from a viral infection, but from its consequences.
I therefore consider “post-COVID” to be a better alternative. This term could also emphasize the differences between patients: even if everyone is more or less restricted in their condition and everyday life, the causes can be very different. Lumping all those affected together is then out of the question.
(Dis)Advantages of the study
The new study would be particularly important if a new therapy could be derived from the statistical correlation. This could, for example, help those patients who have increased deposits in their muscle tissue – and are therefore chronically exhausted.
The research group also has the IDO-2 enzyme in mind. This is produced by the body against the coronavirus. It appears to remain active in chronically affected people – and could cause the problems with the mitochondria and protein deposits.
In addition to the difference between correlation and causality, the small group size alone prohibits far-reaching conclusions. 25 patients is far too few to definitively address the topic of long/post COVID. In particular, we have seen within this group that the correlation with amyloid deposits, for example, only applies to around half of those affected.
The other differences found by the research team are even smaller. This means that they are more of a statistical nature and mainly provide indications of where further research and investigation should be carried out. There are certainly enough unanswered and important questions on the subject.
Summary
- The report that the physical cause of long/post COVID has now been found with the protein deposits is false.
- In particular, the statistically increased deposits were not found in all patients, but sometimes only in half or even fewer of those affected.
- This also does not show that long/post COVID is a physical illness; this dualism must finally be overcome: the “psyche” is embodied and the body is in a sense “ensouled”.
- In general, we should finally stop thinking of psychological or psychosomatic problems as “less real”; the opposite is the case: the psychological is much more directly accessible to us in our experience than the physical.
- Patients should not believe the popular statement that there is nothing they can do to change their situation; it is correct that you cannot simply “think away” such a serious problem, but you can almost always contribute to recovery yourself.
- However, individual possibilities should be taken into account and treatment protocols should not be stubbornly followed; this should be a matter of course.
Follow Stephan Schleim on Twitter/X or LinkedIn. Title image: geralt on Pixabay.

